Antibiotics are arguably the greatest tool modern medicine has given us. Thanks to antibiotics, the majority of our population doesn’t drop dead in a matter of days over a minor bacterial infection. However, many medical professionals and health care organizations are arguing that we have gotten too comfortable with antibiotic prescriptions for just about any illness, even if it’s completely unnecessary. In fact, data from the CDC shows that doctors handed out over 251 million antibiotic prescriptions in 2019 alone – which boils down to about 765 antibiotic prescriptions per 1,000 people.
The overuse and misuse of antibiotics is creating a big problem called antibiotic resistance, which is something the CDC is now calling an “urgent global health threat.” Antibiotic resistance basically means that certain types of bacteria are evolving and developing the ability to survive the drugs designed to kill them. Overtime, this will lead to an increased risk of bacterial infections that are nearly impossible to treat and control.
Antibiotic resistance is a widespread and dangerous problem in American nursing homes. Our elderly population has the highest risk of contracting infectious diseases due to their weakened immune systems and unsanitary facilities. The first line of treatment for these nursing home infections is almost always antibiotics. And too many antibiotic prescriptions on an annual basis often leads to severe reactions, illness, and even death in nursing homes.
That’s why so many nursing homes are now implementing the Antibiotic Stewardship Program, which is designed to improve antibiotic decision-making and usage in order to protect patients from antibiotic resistance, reactions, and premature death. Below, we go in-depth about the dangers of antibiotic resistance in nursing homes as well as how each facility can improve antibiotic stewardship for the health and safety of their patients.
If your elderly loved one is suffering from chronic nursing home infections and/or antibiotic resistance, you may have grounds to file an abuse and neglect claim. Call our Chicago elder abuse lawyers at 312-321-1111 today.
What Are Antibiotics?
Antibiotics are drugs designed to treat bacterial infections such as UTI in nursing homes, strep throat, and tuberculosis. Antibiotics don’t treat viruses, like the flu or the common cold. They work by killing and/or stopping the multiplication of harmful bacteria that’s causing the illness. After only a couple days of antibiotic use, patients begin to feel better. Certain antibiotics are designed to kill a certain type of bacteria, while broad spectrum antibiotics are designed to kill a wide range of bacteria.
Before antibiotics, millions of people suffered severe illness and death due to bacterial infections (a classic example: the bubonic plague, caused by the bacterium Yersinia pestis). Now, antibiotics effectively treat infections and extend the average lifespan all over the world.
What is Antibiotic Resistance?
Antibiotics are possibly the epitome of “too much of a good thing can be a bad thing.” In other words, taking too many antibiotics too often can lead to something called antibiotic resistance, which occurs when bad bacteria and microbes evolve and develop the ability to survive the drugs designed to kill them. This can lead to a huge problem of incurable infectious diseases.
Viruses, parasites, and fungi can also become resistant to drugs. This is called antimicrobial resistance. Antibiotic resistance is considered a type of antimicrobial resistance.
What Causes Antibiotic Resistance?
The main causes of antibiotic resistance include:
- Overusing Antibiotics: Taking antibiotics multiple times a year for illnesses that won’t respond to them can lead to the development of resistant bacteria. For example, some bacterial infections are minor and can clear up on their own without the help of antibiotics. Meanwhile, some illnesses like the average sore throat (pharyngitis, a virus) don’t even respond to antibiotics. Frequent, unnecessary antibiotic use like this will inevitably lead to antibiotic resistant bacteria.
- Misusing Antibiotics: Antibiotics are amazing, powerful medications that can make people feel better in a matter of 2 days. Some people take this as a sign to disregard their doctor’s orders and stop taking the antibiotics before their course is over. This is a huge, potentially dangerous mistake. Patients must finish their entire antibiotics course even if they feel better. If not, the bacteria that hasn’t been killed yet will continue to grow and, in many cases, the infection will come right back. Either that, or the infection will be even harder to kill in the future because the bacteria evolved. This is a very common cause of recurrent urinary tract infections.
- Spontaneous Resistance: Sometimes, you can follow your doctor’s exact instructions about your antibiotics and the bacteria will still mutate on its own and become resistant to the drug in the future.
- Transmitted Resistance: It’s very possible for people to have an infectious disease that’s become resistant to antibiotics and pass on that same bacteria to someone else. This means that this person will become infected with the same antibiotic resistant bacteria.
How Many Antimicrobial-Resistant Infections Occur Each Year?
More than 2.8 million antimicrobial infections occur in the United States alone every year according to the Centers for Disease Control (CDC). These infections result in 35,000 American deaths every year. Meanwhile, the worldwide annual death toll for antimicrobial resistance is around 1.27 million.
Over the last 5 years, the CDC stated that infection prevention and control efforts helped reduce these types of infections by 30% in hospitals and 18% in the community. However, the COVID-19 pandemic almost entirely erased this progress.
Common Antibiotic Resistant Bacteria
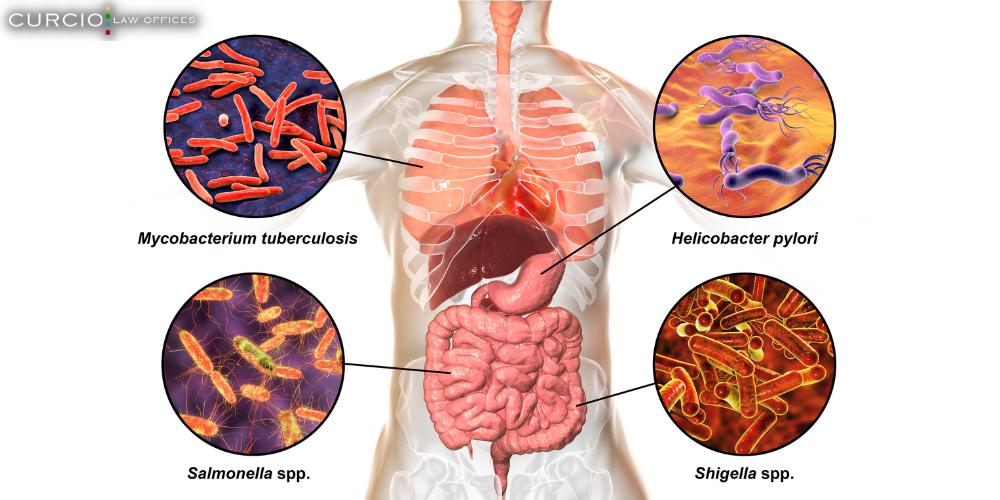
There are many antibiotic resistant bacteria out there, but the most common ones are:
- C. diff (Clostridioides difficile) – a bacteria that causes diarrhea and/or colitis. It occurs when the healthy gut microbiome is disrupted, usually due to frequent and unnecessary antibiotic use.
- Methicillin-Resistant Staphylococcus Aureus (MRSA) is a type of staph bacteria that causes a skin infection. It’s one of the most difficult infections to treat and can even be deadly.
- Gonorrhea is a sexually transmitted disease (STD) that can lead to infertility if not treated quickly and correctly.
- Tuberculosis, also known as consumption, is an incredibly dangerous lung disease that killed around 4 million Europeans in the 19th and 20th centuries. Now that tuberculosis is preventable and curable, people believe the illness is a thing of the past. However, thousands of people still contract and die from tuberculosis every year, especially since the bacteria is resistant to many types of antibiotics.
Many of these bacterial infections are actually referred to as “superbugs” because they’re resistant to several types of antibiotics and other drugs. Therefore, superbugs are incredibly dangerous and often deadly, especially among the elderly and chronically ill population.
Complications of Antibiotic Resistance
Antibiotic resistance is an “urgent global health threat” according to the CDC. It leads to increased cases of both infectious disease and death, especially among vulnerable parts of the population. Aside from that, antibiotic resistance can also lead to:
- Serious adverse effects, such as organ failure, from second and third line medications
- More strain on our global healthcare system
- Higher medical costs
- Longer hospital stays and more medical appointments
- A general loss of control over public health threats
In order to combat antibiotic resistance, medical professionals are turning their efforts towards increased infection prevention measures and responsible antibiotic use.
The Growing Problem of Antibiotic Resistance in Nursing Homes
According to the Centers for Disease Control and Prevention (CDC), 70% of nursing home residents are prescribed one or more courses of antibiotics every year, making them the most frequently prescribed medication in nursing facilities. Not only that, but the CDC claims that between 40% and 75% of antibiotic prescribing in nursing homes is inappropriate or unnecessary. With these startling statistics, it’s no surprise that antibiotic resistance is a very common and dangerous problem among nursing home residents.
These nursing home residents have weakened immune systems due to their age and other health conditions, so they have an increased risk of contracting serious infectious diseases, such as urinary tract infections (UTIs), MRSA in nursing homes, gastrointestinal infections, and COVID-19 in nursing homes. This is especially true if nursing homes abuse and neglect their residents by practicing poor hygiene in nursing homes. Because nursing homes are so quick to prescribe antibiotics for every single infection, thousands of residents are suffering from antibiotic resistance, health complications, and preventable/premature death.

What is the Antibiotic Stewardship for Nursing Homes?
The growing problem of antibiotic resistance in nursing homes led to the creation of antibiotic stewardship programs for U.S. nursing homes.
An antibiotic stewardship program is designed to optimize antibiotic prescribing and usage in order to reduce the number of antibiotic resistant infections and their associated complications in nursing facilities. These programs are basically antibiotic guides and toolkits made up of 7 core elements to promote optimal patient care and patient safety.
Core Elements for Antibiotic Stewardship in Nursing Homes
In order to best combat antibiotic resistance, nursing homes must follow the following 7 elements: leadership commitment, accountability, drug expertise, taking action, tracking and reporting antibiotic use, and education.
Leadership Commitment
The first element of antibiotic stewardship programs is leadership commitment. This means that nursing home leaders must commit to optimized antibiotic decision making and usage.
Nursing home leaders are encouraged to show support towards the stewardship in the following ways:
- Writing statements to staff, residents, and families about improving antibiotic prescribing and usage.
- Ensuring that nursing home employees are assigned stewardship-related duties.
- Communicating with nursing home employees about antibiotic prescribing expectations as well as the enforcement of stewardship policies.
- Promoting and improving antibiotic stewardship policies through education and enforcement.
Accountability
The next element in antibiotic stewardship programs is accountability. The goal here is to hold certain nursing staff accountable for their role in improving antibiotic resistance. Nursing homes should empower and assign duties to the medical director, nursing director, the consultant pharmacist, infection prevention program coordinator, and the consultant laboratory.
Drug Expertise
Drug expertise is another important element in antibiotic stewardship programs. This means employing the help of medical professionals (such as consultant pharmacists) with extensive knowledge of antibiotic and antimicrobial resistance to help reduce the unnecessary use of these drugs.
Taking Action to Improve Antibiotic Use
Now it’s time for nursing homes to take action. Nursing staff members must implement improved antibiotic prescribing policies as laid out by the CDC and the Centers for Medicare and Medicaid Services (CMS). For example, nursing staff should improve the evaluation of bacterial infection symptoms, optimize diagnostic testing, and follow an antibiotic review process.
Tracking and Reporting Antibiotic Use and Outcomes
Just like anything else, improving antibiotic and antimicrobial use in nursing homes is going to involve some trial and error. That’s why nursing homes need to closely monitor data regarding antibiotic prescribing policies but also data regarding the effectiveness of these policies thus far. For example, nursing staff members should track and report:
- How and why antibiotics are prescribed to residents,
- How often and how many antibiotics are prescribed to residents,
- And any adverse or improved outcomes from antibiotic prescriptions.
This allows nursing staff members to see any shortcomings and ways to improve antibiotic stewardship.
Education
Possibly the most important part of any nursing home antibiotic stewardship program is education. All nursing staff members, clinical providers, residents, and resident’s families need to be fully informed of not only the dangers of antibiotic resistance, but the importance of an antibiotic stewardship program. This can be done through e-newsletters, flyers, interactive workshops, etc.
Antibiotics are crucial for disease prevention and treatment. These drugs save and prolong lives. If too many residents contract antibiotic resistant bacteria, nursing staff have far fewer medical options available to protect and treat chronic diseases across the entire facility. It’s crucial for everyone to understand the gravity of this situation.

Call Chicago Elder Abuse Lawyers at Curcio & Casciato Today
If your elderly loved one has suffered from countless nursing home infections which has led to major health complications and antibiotic resistance, you may have grounds to take legal action. Back-to-back nursing home infections can be a sign of poor hygiene as well as abuse and neglect. Our elderly population doesn’t deserve to live their final years in pain due to poor nursing home conditions and health care. Sadly, this is often the reality for our elderly loved ones. Chicago nursing home abuse and neglect lawyers at Curcio & Casciato want to change this reality one civil suit at a time. Call 312-321-1111 to schedule a free consultation with our legal team today.



